16 April, 2014
There are three main challenges to achieving effective wound surveillance. These challenges are:
- obtaining accurate measurements and reliable healing trends;
- managing image quality and logistics; and
- gathering standardized documentation.
Dimension One: Measurement
Practitioners measure wounds to identify a healing trend, usually area reduction over time [i]. They rely on this trend information to predict healing rates, identify factors delaying healing in a timely fashion, intervene rapidly, and provide appropriate treatment
Unfortunately, not only are methods commonly used in clinical practice difficult to use, they are often poorly validated, and subject to serious question in terms of accuracy and precision [ii]:
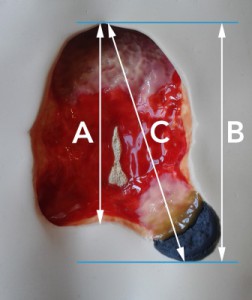
- Rulers: The standard area formula length x width is inaccurate, and typically over-estimates true wound area by 44% [iii]. This method is also not precise, with practitioners often using different ways to calculate length and width, resulting in measurements with poor reproducibility (Figure 1);
- Planimetry, such as tracing a wound onto acetate film and calculating the area, has been estimated to have an up to 22% error rate [iv];
- Digital planimetry, which involves using software to estimate the area within a user-drawn outline on a digital image, requires a number of conditions to be met to ensure accuracy is not compromised. For an ideal outcome, the wound must lie in a flat plane; a scaled calibration target, such as a ruler, must be in a plane; the wound and the target must be in the same plane; the camera lens must be parallel to the wound and the target; and the target must be identified accurately. For instance, slightly altering the angle of the camera so it is no longer perpendicular to a wound can distort measurements by 10% [v] to 35% [vi];
- Geometry: Errors compound on any method that involves determining an area based on a linear measure. This not only involves rulers, but also digital planimetry.
- Wound depth and volume measurement are even more problematic. For instance, wound volume measured using alginate casts produces errors of 5%-40% [vii], and the Kundin method is considered to be very subjective [viii].
Imprecise trends
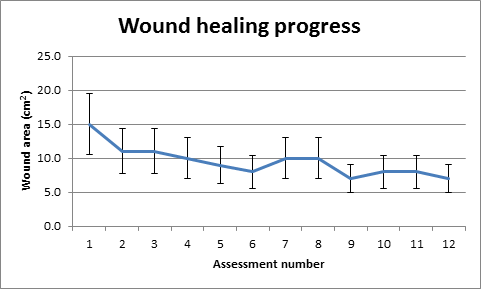
The next step is for practitioners to graph the measurements they have made over time in order to look at healing trends. Many practitioners assume that wound measurements contain a systematic (non-random) deviation from the true value – in other words, they are “uniformly inaccurate”, and can therefore form a trustworthy healing trend. However, this is not the case. As wounds are measured by many assessors, the inaccuracies are random, making the resulting error bars of their measurements too wide to be clinically useful. Rating variability ranges from 16% to more than 50% [ix],[x].
There seems to be widespread acceptance of inaccuracy without an acknowledgment of its adverse implications for clinical practice. Figure 2 shows how lack of precision in healing trend data can affect clinical decision making. If error bars are too broad to confirm if a wound is getting smaller or larger, a facility is less able to detect and respond promptly to meaningful changes in wound size, or to provide valid evidence supporting healing outcomes.
Practitioners skilled at wound care combine their measurements with clinical judgment about the wound to assess change and make sound decisions. However, the healthcare system is moving towards higher levels of precision, demanding not just quality care, but evidence of quality care.
Precise measurement is important, and inaccuracy is costly. It has been estimated that the measurement-related portion of the US healthcare budget ranges from 10%-15%, and error-related spend (re-work, quality tests, etc.,) accounts for 30% [xi]. As technology developments make measurement in healthcare easier and more precise, payers can demand more accurate measurement data as a basis for reimbursement and shift the costs of inaccuracy to providers. Wound measurement is not exempt from this trend.
|
What is the area of this wound?
Figure 1: There are different methods for making length and width measurements – such as (1) the longest length and largest perpendicular width method; and (2) the so-called clock method which requires a superior to inferior (or 12 o’clock to 6 o’clock) measurement, and a medial-lateral (or 3 o’clock to 9 o’clock) measurement. But even when people are using the same method, they can obtain very different results. For example, if the clock method is used, the length chosen may be the longest distance in the superior-inferior direction (A), or the length of the extent of the wound in the superior-inferior direction (B). Or – even though practitioners are trained not to do this – they often tilt the measurement from the strict 12 o’clock-6 o’clock orientation (C). In this example, the largest length is 15% longer than the shortest. |
|
Figure 2: Clinical decision-making is adversely affected by measurements with large errors and the resulting imprecise trends that are based on those measurements. For instance, if the error rate on a weekly assessment is ±30% as shown above, and the wound is making a 10% change each week, it will take three weeks before any improvement or deterioration can be objectively proven. Note that in this example, deterioration and improvement in the wound are undetectable between assessments 2 and 12. |
Dimension Two: Wound Imaging
Images are useful for wound documentation. However, if the images are neither standardized nor of high quality, they add risk and introduce error to the documentation. Wound photo transfer can cause local storage and security issues and photos are difficult to transfer to an electronic medical record (EMR). Guidelines are often complicated, and the cost of ownership of cameras can escalate.
Shaw and Bell sum up the drawbacks of digital photography: “Digital imaging takes considerable time and studies seldom show the total time to capture the image, transfer the image from the camera to the computer, and then calibrate and measure the wound… Many additional factors also require management such as lighting, environment and the distance of the camera from the [foot].” [xii] A busy nursing team with high turnover and multiple demands would struggle to deliver consistently high quality images under these conditions.
Dimension Three: Documentation
The problems described above are compounded by the ineffective and inefficient collection and management of critical information about wounds. While there is a lot of literature about “wound management” in the context of clinical guidelines, very little has been written about the complexity of the overall wound management effort. Systemic factors include:
- Risk management: Many quality, risk and legal managers have experienced the headache of putting together pieces of ad hoc documentation when there is an adverse event such as a hospital-acquired pressure ulcer. With the spotlight on a potential legal case or penalty, the lack of standar dization of wound documentation is exposed and there is a higher risk of an unfavorable outcome [xiii]. Practitioners are not necessarily adept at gathering accurate measurement data or conforming with strict documentation standards, resulting in different interpretations of measures or levels of reporting [xiv].
- Multi-disciplinary team communication: It is being recognized that success in chronic wound care requires an integrated chronic disease management methodology [xviii] rather than siloed thinking. Disciplines involved in the wound care effort may include nursing, nutrition, occupational therapy, orthotics/prosthetics, physical therapy, general practice, podiatry, social work, pharmacy, and specialists [xiv], often in multiple organizations. Under these circumstances, care teams need high-quality communication based on readily available wound information that is accurate, easy to access, and comprehensive.
- Lack of specialist competency: There are recognized issues with the accuracy of wound assessment by non-specialized staff [xv]. This extends to treatment decisions. In a retrospective analysis, 78.5% of patients treated by a board certified wound care nurse healed in comparison to the 36.3% of those treated by non-certified nurses [xvi]. Wound specialists are a crucial part of the wound care system, but are typically stretched to capacity managing the wound care effort and an increasing documentation burden. Often, they are required to travel to patients, further consuming time and effort [xvii]. The consequences of this disparity of skill include unnecessary patient suffering, readmissions, penalties and litigation risks, rework and extra costs. For instance, hospital admissions and extended hospital stays typically consume 37%-49% of the total cost of wound care [xviii].
- Litigation: Up to 20% of all US legal medical claims and more than 10% of settlements are wound related[xx], and there are more than 17,000 pressure ulcer-related lawsuits filed annually in the United States [xix]. Settlements average $279,000 each [xx]. Documentation is a critical success factor in pressure ulcer litigation [xxi]. If documentation can prove no neglect occurred, a lawsuit is less likely to proceed; however, many out-of-court settlements have been forced on providers because of a lack of evidence of care, not necessarily the absence of care itself [xxi].
The solution: innovation
Practitioners use information to help make decisions that improve the quality of care, and to fulfil their administrative obligations. The regulatory changes in wound policies and the need for accountability and proven outcomes justify a new approach to wound surveillance.
Traditional wound measurement modalities result in measurements with large errors and unreliable trends. However, three-dimensional methods can accurately measure area, along with the important indicators of depth and volume. Until recently, these systems were prohibitively expensive and cumbersome, but there are now commercially-available three dimensional (3D) measurement systems that overcome many of the limitations of traditional wound measurement techniques. Such 3D systems account for both the curvature of the body and the irregular nature of wounds. Therefore, accurate measurements can be taken from the 3D models that these systems generate.
These systems do, however, share some of the limitations of traditional techniques. For example, surface-based 3D systems cannot quantify the degree of undermining or tracking in a wound. Circumferential wounds can be difficult to assess, although some systems do allow for accurate measurements of extensive wounds [xxvi].
3D systems do not offer diagnoses or replace good clinical judgment; rather, they equip an organization to achieve better wound outcomes by supplying precise measurement and trend data, and supporting more effective wound surveillance and communication between wound stakeholders.
One such 3D-based system is the Silhouette® wound imaging, measurement and documentation system.
To find out more, click here.
[i] Gottrup F., (chair). Outcomes in controlled and comparative studies on non-healing wounds: recommendations to improve the quality of evidence in wound management. Journal of Wound Care June 2010;19(6)
[ii] Flanagan M. Improving accuracy of wound measurement in clinical practice. Ostomy Wound Management. 2003 Oct;49(10):28-40.
[iii] Romanelli, M. MD, PhD: Wound assessment: Clinical and instrumental (presentation), Wound Healing Research Institute, Department of Dermatology, University of Pisa (2006)
[iv] Shaw, J, Bell, P. Wound Measurement in diabetic foot ulceration, from Global Perspective on Diabetic Foot Ulcerations”, edited by Thanh Dinh, ISBN 978-953-307-727-7 December, 2011: under CC BY 3.0 license
[v] Mayrovitz, H. Documenting wound areas via digital photography: effect of camera angle on area accuracy, Presented to WOCN Society 40th Annual conference, June 2008.
[vi] Rennert, R, Golinko, M, Kaplan, D, et al. Standardization of wound photography using the wound electronic medical record. Advances in Skin and Wound Care 22(1).
[vii] Plassmann, P, Jones, T. MAVIS: a non-invasive instrument to measure area and volume of wounds. Medical Engineering & Physics, July 1998;20(5):332-338
[xiii] Richard, J, Daures, J, Parer-Richard, C, et al. Of Mice and Wounds: Reproducibility and Accuracy of a Novel Planimetry Program for Measuring Wound Area. Wounds. 2000;12(6)
[ix] Wendelken, M., et al: Wounds Measured From Digital Photographs Using Photodigital Planimetry Software – Validation and Rater Reliability. Wounds. 2011;23(9):267-275
[x] Koel, G. Reproducibility of current wound size surface measurement, Conference proceedings, EWMA, May 2008
[xi] May, W. E-Health and Technology: Empowering Consumers in a Simpler, More Cost Effective Health Care System. Before the Committee on Commerce, Science, and Transportation, Subcommittee on Science, Technology and Space, United States Senate. July 2001,
[xii] Shaw and Bell. Wound Measurement in Diabetic Foot Ulceration (2011)
[xiii] Bicandi, C, Hawkins, M. When Bad Pressure Ulcer Documentation Happens to Good People. Presented at Idaho Health Care Association – Idaho Center for Assisted Living 46th Annual Convention & Tradeshow, January 2012
[xiv] The Health Foundation (editorial) http://www.health.org.uk/news-and-events/newsletter/measuring-quality-a-complicated-task/ Accessed 02/20/2014
[xv] Hurd, T. Understanding the financial benefits of optimising wellbeing in patients living with a wound. Wounds International, June 2013;4(2)
[xvi] Zulkowski, K. ‘Assessing Your Pressure Ulcer Knowledge’ WoundSource, Dec 2012 http://www.woundsource.com/blog/assessing-your-pressure-ulcer-knowledge
[xvii] Khan, A. Pressure ulcer prevalence: hospital-wide monitoring and management. http://www.woundcarenurses.org/uploads/7/6/6/7/7667574/pressure_ulcer_prevalence.pptx (presentation). Accessed 02/20/2014
[xviii] Henderson, K. The ‘rapid track’ to improved wound outcomes. Today’s Wound Clinic, October 2012: 24-25
[xix] Rosenfeld, J. Legal Perspectives: The Significance of Charting in Litigation Involving Pressure Sores. August 2012. http://www.woundsource.com/blog/legal-perspectives-significance-charting-litigation-involving-pressure-sores
[xx] Nixon, M, Rivett, T, Robinson, B. Assessment of accuracy and repeatability on wound models of a new hand-held, electronic wound measurement device Presented at the Symposium for Advanced Wound Care (SAWC), Atlanta, Georgia, 2012.