14 December, 2015

John and Wound Care District Nurse Sara Best discuss a Silhouette wound assessment. (Patient and nurse consents held on file.)
How accurate wound information and images empowered one patient in a healing partnership with his multi-disciplinary team.
John Moles and his wife were settled into retirement, when John was diagnosed with a spinal abscess resulting in paraplegia. Their life was thrown into a dramatic new chapter.
John was admitted to a specialist spinal injury rehabilitation hospital dedicated to teaching its patients independence. On discharge from the rehabilitation unit, John was transferred to a residential care facility as a temporary measure while suitable accommodation and assessment of care needs were organized.
His wife sold their multi-storey home in favor of a suitable apartment, and after many months the couple was looking forward to their “new normal”. Unfortunately, a month before the final transition to the apartment, John developed a Stage 4 pressure injury to his left ischial tuberosity.
Due to the extent of the injury, it was not possible for John to go home. The impact of the diagnosis was profound: John commenced total bedrest in the residential care facility as the marathon effort to heal the wound began.
The debilitation wrought by the wound surpassed that of the paraplegia, he says. “I began to have doubts about my ability to live life independently. I had to be repositioned every three hours which I couldn’t do on my own. I was totally reliant on other people.”
John was on bedrest for almost a year in the residential care facility, during which time he had just two outings. “I had to beg to be off bedrest for five hours at Christmas,” he says.
“One thing I can do is try to help people trying to help me. Objective information helps me to understand what needs to be done and why.”
John Moles, pressure ulcer patient
John notes how debilitating the ulcer was. “It’s bad enough being paraplegic, but at least I had some freedoms. Before the injury put me on bedrest I could at least go to the coffee shop every day, chat with people. It’s those types of things you take for granted, even as a paraplegic. Once I had a chronic wound, that was that. I was terribly reliant on visitors. It robbed me of my independence.”
Navigating the healing journey
But John’s experiences of paraplegia had taught him empowerment and determination, and his ammunition was information.
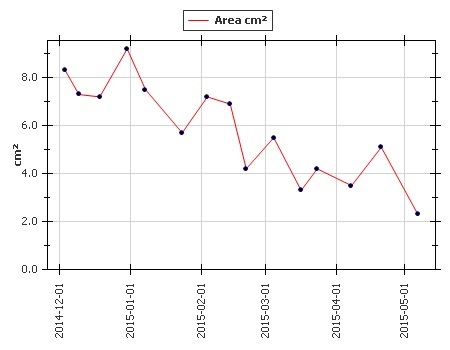
Silhouette’s accurate healing graph shows John’s roller-coaster route to getting his pressure ulcer under control. (Patient and provider consent held on file.)
At the centre of a multi-disciplinary team, John actively entered a partnership with a wound care team dedicated to his healing. The goal was his return to his wife and home. His wound nurses assessed his wound using the Silhouette wound assessment and information system, which presented objective imaging, measurement and healing trend information. This information became the navigation chart they used to traverse the healing journey.
Silhouette’s imaging and measurement helped John to become acquainted with his wound and its behavior. During his months of bedrest, John avidly followed the images that Silhouette presented of his wound’s healing progress. “It was the fact that you could get accurate measurements of the extent of the wound. It gave an indication of whether the wound was improving or not,” he says.
Navigating the healing journey
While on bedrest, John diligently followed the instructions of his care plan, determined to support the healing process so he could reach his goal of living in the apartment with his wife. “With the right information, if you understand what the care team is trying to achieve, you can understand the pros and cons and play your part,” he says.
John also observed Silhouette empowering the multi-disciplinary team. Silhouette images provided the evidence the team needed to enable a hospital admission when necessary, and to advocate for the medical necessity of his advanced treatment regime.
“Silhouette made it easier for all the people who were dealing with me to understand the whys and wherefores of my wounds, to alleviate the problem and devise a solution,” says John.
The care team was extensive, guided by the wound specialists and supported by personnel in the residential care facility, John’s GP, physio- and occupational therapists, and dietician. Silhouette information kept them all on the same page with a clear point of reference supporting the care plan and helping them tackle unexpected issues, such as infection and numerous other setbacks.
After seven months of bedrest and close monitoring, John’s wound had recovered sufficiently to be considered for remedial plastic surgery. This was successful and, four months later, John finally returned home. His wounds, now at a manageable level, are closely monitored by the district nursing team.
John says the objectivity of Silhouette’s information has given everyone in the care team confidence, providing a central, reliable point of reference. The GP supports John when extra treatment is required, with reference to the care team and Silhouette information. This provides vital continuity.
Accountability and partnership
Silhouette’s information empowers John and makes clear the rationale for his care plan, to which he keeps his caregivers accountable. “If I know what’s going on, I can monitor my own progress. I tell the carers to report any change in my skin condition; most let me and the [specialist wound] nurse know straight away if there’s a change. I have trained the carers,” he says.
John and his wife are again regulars at their local café, and the apartment provides a base from which he can engage with the world. His partnership with his multi-disciplinary team continues.
“There are some things I can’t do for myself, but one thing I can do is try to help people trying to help me. Objective information helps me to understand what needs to be done and why.”
NB: Patient and practitioners’ consent held on file.