26 June, 2020
With the help of Silhouette, a wound care nurse was able to collect the information she needed to prove that changes to traditional wound-healing practices could improve the outcomes for her patient with Epidermolysis Bullosa (EB).
Silhouette proves that a change in practice can significantly improve healing and reduce discomfort for EB sufferers
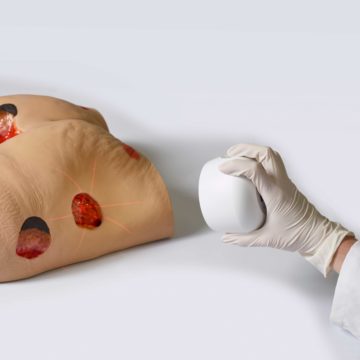
EB is a rare genetic condition caused by a missing collagen protein that affects the skin’s connective tissues. People with EB have very delicate skin that blisters and tears easily, and in severe cases the slightest touch can cause blisters or leave burn-like wounds. Occurring in an estimated 1 out of every 50,000 live births globally, EB does not discriminate—it affects every racial and ethnic group and both sexes equally.
People with EB are also more susceptible to squamous cell carcinoma (SCC) which spreads at a much faster rate that for those without EB, so any SCC needs to be dealt with urgently.
The standard treatment for SCC is to remove the affected skin and cover the wound bed with a skin graft from another site on the patient. For people without EB, the skin graft is shown to help the wound bed heal faster, however, for a person with EB skin grafting creates another wound on their body that can be just as difficult to heal as the SCC site.
A New Zealand based EB Clinical Nurse, Mo Blishen, started looking for alternatives to skin grafting for one of her EB clients with SCC to reduce their discomfort. Ms Blishen says, “I wanted to try using a collagen substitute instead of the patient’s skin to cover the wound bed. However, before I could even suggest a change in practice, I needed to provide evidence that using a collagen substitute over a skin graft would make a real difference for the patient.”
To change the way patients are cared for there needs to be evidence that the change (whether it is a new practice, procedure, or product) will result in positive outcomes for the patient. So, before adopting any new approach to care, it must be thoroughly researched and there must be evidence to prove that the change is working and worth adopting.
With the help of the Silhouette wound assessment system, Ms Blishen was able to collect the information she needed to present her case. Using a collagen substitute for her EB patient’s biopsy wound, she tracking the wound’s healing progress over a 4 week period. She gathered images and measurements every 2 days when the dressings were changed.
“With Silhouette, I was able to accurately map the changes in the wound and show that the wound could heal well without a skin graft. I was able to provide accurate measurements and report on the viability of using the collagen substitute in an easy to read and see format. Silhouette provided me with the objective information that I needed to present to the surgeon and prove that a skin graft was not necessary for wound healing in this case.”
Surgeons working with EB patients with SCC can now feel comfortable only removing the affected area of skin and leaving the wound for the EB nurses to monitor and heal (which may include a collagen substitute) without the need for taking an additional skin graft from another part of the patient’s body and causing more damage and discomfort. “This change in how we heal SCC wounds for EB patients makes a real difference to the patients and their quality of life,” says Ms Blishen.
Ms Blishen and her team of EB nurses continue to use Silhouette to keep track of any suspicious areas of their patients’ skin. She says, “We are also able to monitor how different dressings and regimes work with individual clients as what works for one does not necessarily work for another. Having the ability to show the development of suspicious wounds and getting them seen in time could honestly be the difference between life and death—it’s a game-changer.”
Doc Number: 2020-00086