2 July, 2014
By Mark Nixon, MD, Chief Medical Officer, ARANZ Medical Ltd
Non-specialists’ inaccuracy has been identified as the most significant wound surveillance concern for wound stakeholders in a recent online survey.
 The ARANZ Medical survey of 100 WoundSource subscribers between 19 April and 19 May 2014 found that 61% of respondents’ facilities have identified wound surveillance improvement as an active priority for 2014. The participants took part in the survey in conjunction with an ARANZ Medical-sponsored white paper distribution exploring the various dimensions of evidence-based wound surveillance.
The ARANZ Medical survey of 100 WoundSource subscribers between 19 April and 19 May 2014 found that 61% of respondents’ facilities have identified wound surveillance improvement as an active priority for 2014. The participants took part in the survey in conjunction with an ARANZ Medical-sponsored white paper distribution exploring the various dimensions of evidence-based wound surveillance.
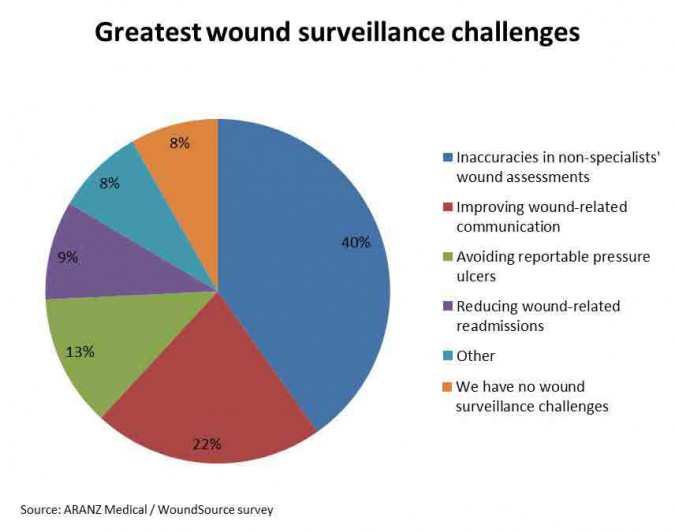
Almost 40% of respondents identified “inaccuracies in non-specialists’ wound assessments” as their top challenge in wound surveillance. The next most pressing challenge was “improving wound-related communication” (21%), followed by “avoiding reportable pressure ulcers” (12%). Less than 10% said they have no wound surveillance issues.
More than half (53%) of the respondents had specialist or WOCN roles. A further 22% of the respondents had general nursing roles.
Respondents with administrative responsibilities were more likely than nursing respondents to identify the reduction of wound-related readmissions and avoiding reportable pressure ulcers as major issues. Three out of six respondents at chief executive level identified wound-related readmissions as the key challenge, as did three out of six clinical coordinators. However, at director level, half agreed with nurses that non-specialist inaccuracies were the key wound surveillance issue.
One-third of respondents were based in acute hospital settings, mostly in wound specialist/WOCN roles. Around half of these identified inaccuracies in non-specialists’ wound assessments as the major challenge, followed by avoiding reportable pressure ulcers and wound-related re-admissions (12% of acute facility respondents for each issue).
The next most common care setting surveyed was home health. For these respondents, improving wound-related communication and inaccuracies in non-specialists’ assessments were of equally high concern (37% each in the home health category).
Of the eight respondents from LTAC settings, most identified non-specialist inaccuracy as the key concern.
Around 80% of the respondents were from the United States.
Respondents with administrative responsibilities were more likely than nursing respondents to identify the reduction of wound-related readmissions and avoiding reportable pressure ulcers as major issues.
Leverage WOCN expertise using technology
There are recognized issues with the accuracy of wound assessment by non-specialized staff. Wound specialists are a crucial part of the wound care system, but are typically stretched to capacity managing the wound care effort and an increasing documentation burden. Often, they are required to travel to patients, further consuming time and effort. The consequences of this disparity of skill include unnecessary patient suffering, re-admissions, penalties and litigation risks, rework and extra costs.
Innovative technologies offer a solution. As wound surveillance innovator Kathy Deck, RN, CWON, wound specialist at Barlow Respiratory Hospital in Los Angeles, explained in a recent case study, it is possible to leverage wound specialists’ knowledge to improve wound performance across a facility, and lift the assessment capability of non-specialists using the right technology.
“Other entities only have one set of eyes that can’t monitor everything. With [3D wound surveillance], I can see what’s going on – it’s as if I am overseeing the wound care program with 100 pairs of eyes and accurately capturing what’s really going on.”
Next steps
It is clear that facilities are concerned about the consequences of inadequate wound assessment and wound documentation practices. Read this white paper, which delineates some of the issues and explores an innovative approach to help achieve accurate, comprehensive wound surveillance.
Document number: 2014-00213