Chronic wounds affect millions of people each year, causing a significant reduction in patients’ quality of life, placing a huge burden on the healthcare system, and accounting for billions of dollars spent annually in the US. Venous, diabetic and pressure ulcers are the most common types of chronic wound.
An estimated 2% of the United States general population suffers from chronic, non-healing wounds. The cost of caring for these wounds is estimated to exceed $50 billion every year. The prevalence rate is comparative to that of heart failure, but unlike heart failure, little is known about the effectiveness of the treatments and the eventual outcomes that patients with chronic wounds are achieving.
Many wound care practitioners are using continuous wound measurement and monitoring to make better treatment decisions and thereby improve patient care and outcomes. The main advantages of continuous wound measurement are shown in the following table.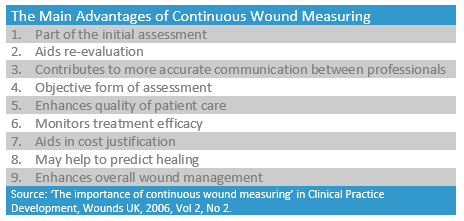
An effective wound management approach involves:
- obtaining an accurate baseline and ongoing measurements,
- utilising a transparent and standard process, and
- using the information gathered to guide better treatment decisions.
These three elements are discussed further below, demonstrating how accurate information on wound healing progress can provide medical and economic benefits for both patients and wound care providers.
Accurate Baseline and Ongoing Measurements
Evaluating and recording wound details, such as size and volume, is a routine aspect of patient assessment and provides ongoing information on healing. The characteristics that the Wound Healing Society recommends recording include location, staging, size, base, exudates, infection condition of surrounding skin and pain. They also recommend evaluating the wound healing rate to determine if the treatment is optimal.
It is very important that an initial, accurate wound assessment is completed to provide baseline data about the status of the wound and valuable information that can assist in identifying the short and long term goals of care. If not accurately completed, the treatment may not be as successful, drawing out the healing process, costing the hospital and care facilities more, and negatively impacting on the patient’s quality of life.
Transparent and Standard Processes
Wound measurements that are completed and recorded in an accurate and methodical manner ensure the usefulness of the data for other wound care practitioners and help to improve the outcomes for the patient. When wound measurement is accurately undertaken as part of the assessment process, it allows wound care practitioners to draw comparative results and analyse the treatment regimens over time. Plotting the healing rates of wounds against the initial wound area and then comparing them with a defined standard helps to inform clinical decision-making and reduces the likelihood of ineffective treatments. Having the tools to easily and accurately document the wound information for later referencing is an important part of this process.
Usually, there are a variety of different doctors, nurses, surgeons, specialists, and other healthcare professionals involved in the treatment of a wound and through the continuum of the patient’s care. When wound measurements are completed using the same technique, accurately and methodically, there is consistency in the information that can be shared from practitioner to practitioner. Communication also needs to be interdisciplinary due to the nature of the care team for wounds. Different health care providers need different information and will interpret information in different ways, so it is important that the information that they are given is accurate, clear and timely. A transparent and straight-forward trail of information about the changes in a wound over time is made even more useful when images are attached. A clear image of a wound makes communication between practitioners easier, conveys the status of the wound in under a minute, and avoids the need to spend an hour or longer describing complex wounds in note form.
Barlow Respiratory Hospital, a long-term acute care hospital network in Los Angeles, is streamlining their documentation processes and improving their assessments, communication, and patient outcomes with Silhouette. Kathy Deck, Wound Care Specialist (RN, CWOCN) at Barlow Hospital, says “with Silhouette, I can see what’s going on – it’s as if I am overseeing the wound care program with 100 pairs of eyes and accurately capturing what’s really going on.” Read More
Information to Guide Treatment Decisions
Having the ability to predict the healing of wounds via different courses of treatment can help ensure the right path is taken. Knowing at the different points of assessment exactly what has happened up to that point with the wound, and being able to plot out the ongoing trend of the wound dictates the course of treatment to be taken. The key to doing this successfully is through continuous monitoring in the changes to the wound size.
Early detection of poor healing wounds will aid in the management of resources by identifying those who will benefit the most from more intensive and costly treatment. More importantly, by preventing the use of ineffective therapies, the number of days an ulcer exists will decrease. This can have several implications, including improving the patient’s quality of life, reducing the amount of days spent in a hospital, and reducing the chance of complications.
In several clinical studies (e.g. Kantor and Margolis, 2000) it has been shown that percentage change in the size of the wound as it heals is a good indicator for eventual healing. A wound that increases in size by 3% or more at week four had a 68% probability of not healing. Whereas a wound that increases in size by less than 3% or decreases after four weeks had a 75% chance of healing by 24 weeks.
Predicting wound healing is especially important in the current managed care environment in which cost-containment and the need for referral to a specialist have assumed great importance. If further referral and investigation are warranted then the measured wound area is an important piece of medical information.
Conclusion
By accurately undertaking wound measurements and having this information readily available for all parties involved in the wound treatment, the overall quality of wound care will increase for both the patient and the provider.
The provider, who interacts with a wide range of different professions and touchpoints in the healing process, has the necessary information available to more accurately predict the right course of treatment. Having accurate and consistent information also ensures smoother communication between the different treating parties. See how Barlow Respiratory Hospital, a long-term acute care hospital network in Los Angeles has been able to improve patient outcomes through better information.
The patients receive better treatments, which help to heal their wounds faster, and they spend less time in hospital than they would have previously. Predictive healing models mean that changes to the course of treatment can be made early which can streamline their hospital stay or could even prevent them from being admitted in the first place. Accurate wound measurement also lessens the chance of complications that a patient may face, such as infection, lack of progress or even in serious cases, amputation.
The implications for hospitals practicing continuous monitoring of a wound are significant. Regular assessments involving quantifying and documenting wound healing progress are currently the only way of determining treatment effectiveness, guiding further treatment decisions and objectively justifying more aggressive and expensive treatments. The wound assessments enable practitioners to follow a treatment for an optimal period of time, reassess and evaluate the effectiveness of the treatment, and then plan for the next stage— continue with the current treatment, recommend a new treatment, or ensure that further investigation and intervention is carried out.
Practitioners should use the best technique available to them when obtaining measurements and use the same method consistently to ensure the most accurate and useful information is available to them. Measuring methods are not interchangeable as each different method will measure and record information in a slightly different way, skewing the results that are being collected. However, the more accurate and precise the wound measurements are, the more practitioners are able to predict wound healing outcomes as early as the fourth week of treatment. Read more about how wound measurement precision can help predict healing outcomes.
Doc Number: 2017-00153